Q & A: Does it matter who the radiologist is that reads my mammogram or other breast imaging studies? Why?
October 25th, 2012- It matters who reads your mammogram. If your study is read by a radiology doctor (radiologist) who practices general radiology or another radiology subspecialty and only reads a few mammograms per week, you are probably not receiving the best care. Yes, the guy is board certified and is licensed by law to read your mammogram. But I am licensed to read all radiology studies as well, even though my specialty is breast imaging. Doesn’t mean I should muddle through interpreting the next brain or shoulder MRI that comes my way.
Q & A: How do I find a “good” breast imaging center? Does it make a difference where I go?
October 24th, 2012- Yes, it matters where you choose to go for your mammogram! The most basic requirement is whether a facility is accredited under the MQSA (Mammography Quality Standards Act). The accrediting body for most states is the ACR (American College of Radiology), which has a list of requirements and tests that facilities must comply with in order for the centers to achieve accreditation. They look at things such as equipment and film quality, radiation dose, credentials of the mammography technologists and of the radiology doctors
Q & A: What if I feel a lump and the mammogram and ultrasound are negative (normal)?
October 23rd, 2012- Never ignore a lump. When you feel a lump and mammogram and ultrasound (also known as a sonogram) are negative, there is still a 2-3 % chance that the lump is cancer. Have your doctor refer you to a breast surgeon. They might want to perform a needle biopsy in the office based on what they feel, or they may advise surgical removal of the lump in the operating room. If the doctor doesn’t test the lump, and you still feel it, seek a second opinion from another surgeon. You know your body better than anyone.
Q & A : Which Tests Are Best? When Should I Start?
October 22nd, 2012If I am at high risk for breast cancer, what imaging tests should I be having each year, starting a what age?
- If you have a strong family history of breast cancer (mother or sister premenopausal), start having your mammogram 10 years younger than the age that relative was diagnosed, OR at age 40, whichever is younger; but not before age 25. For example, if your sister had breast cancer when she was 44, you should start having your mammogram at age 34. If your mother had breast cancer at 60, you would start having your annual mammogram
Q & A: Laws regarding breast density?
October 19th, 2012Why are there laws in some states regarding women receiving their breast density information?
- A wonderful grass-roots organization has been founded by women personally affected by the lack of information given to them regarding the density of their breasts (www.AreYouDense.org), and they are doing everything they can to address this issue for all women. Because of their advocacy, laws have recently been passed in Connecticut, Texas, Virginia, New York and California, requiring that women be informed of their density
Q&A : How can I find out if my breasts are dense?
October 18th, 2012- Don’t be surprised if your doctor does not know much about breast density. As the issue gains traction, the medical community will become more informed over time. For now, it is up to you to find out if your breasts are dense so you can protect yourself from advanced cancer.
Your density information should be in the official report from your mammogram, so ask your doctor for a copy of this report. Do not rely on the form letter you receive from the mammography center; this will not include your density (unless
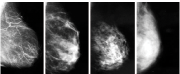
Q & A: What does it mean to have dense breasts?
October 17th, 2012- Breast density is one of the strongest predictors of the failure of mammography to detect cancer. About half of women younger than 50 are dense, and 1/3 of women over 50 are dense. Up to half of breast cancers cannot be seen on the mammogram in women with dense breasts. This leads to missed cancers that are discovered at later stages, resulting in more invasive treatments and a poorer prognosis. 40,000 women in the U.S. die each year from breast cancer. Some of these women had dense breasts and didn’t know it; even though they
Q&A: Does Normal Mean No Cancer?
October 12th, 2012If I have a negative (normal) mammogram, does that mean I definitely don’t have breast cancer?
- Mammography is an imperfect test. A “normal mammogram” report does not mean that a woman does not have breast cancer. Overall, mammograms will pick up 80-90% of cancers. That’s pretty good, but there are still 10-20% of cancers that will not be seen, and will present as an “interval cancer” with a palpable lump.
The cancer detection rate plummets in women with dense breasts to only 40-50% of cancers picked up
Q&A: When and How Often Should I Visit?
October 11th, 2012At what age should I start having screening mammograms, and how frequently? Why does there seem to be controversy in the media surrounding this?
- For most women, age 40 should be when you start having yearly mammograms in order to minimize your likelihood of developing advanced breast cancer. Some doctors send their patients for a baseline mammogram at age 35, and I wouldn’t argue with that.
If you have a strong family history of breast cancer (mother or sister), start having your mammogram 10 years younger
Q&A: Is Digital Mammography More Accurate?
October 10th, 2012What is a digital mammogram? Is it more accurate?
- The traditional mammogram was a film-screen, or analog, mammogram. In 2000, the FDA approved the use of digital mammography units. An x-ray is still taken, but instead of the beam being directly translated onto a film, the beam is converted to digital data that is then processed to appear on a computer monitor. The digital image can be manipulated on the computer screen, with tools for magnification, contrast and windowing adjustments, sharpening, etc. Approximately