The Myth of the Negative Mammogram
It is a scenario familiar to all breast imaging practices.
A patient feels a lump in her breast and calls her doctor. The doctor examines her, agrees that a lump is present, and refers the patient to a breast imaging facility for a diagnostic mammogram and breast ultrasound (also known as a sonogram). At her mammogram appointment, a little sticker is placed on the lump felt by the patient, and mammogram images are taken. Something may or may not be seen on the mammogram at the site of the lump. A breast sonogram is performed, and a suspicious mass is seen, clear as day. And sometimes it’s not so tiny. The yellow arrow in the sonogram image below demonstrates one such mass:
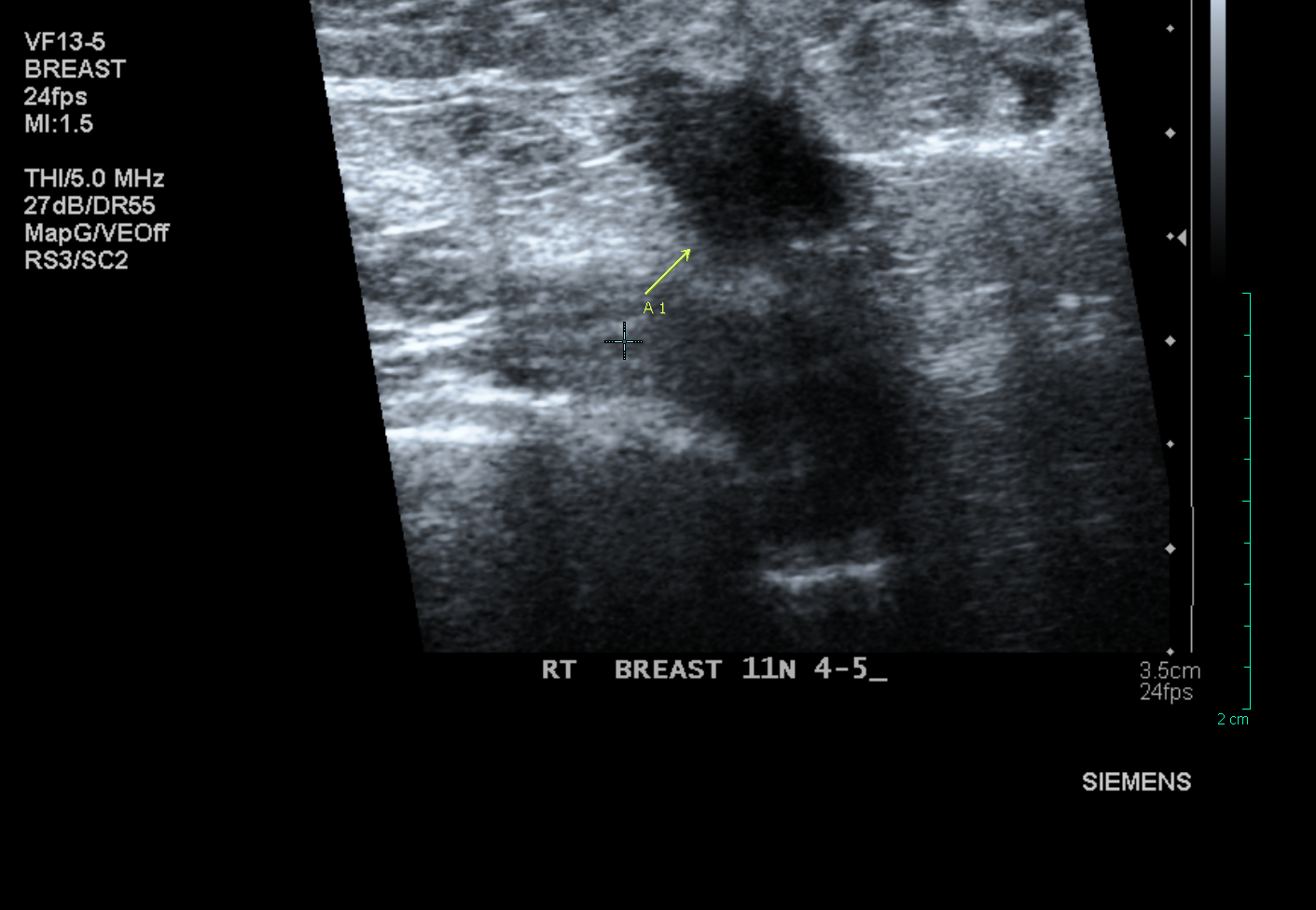
The radiologist assigned to read mammograms that day tells the patient that a mass has been found, and she needs to have a needle biopsy. The biopsy is performed, cancer is diagnosed, and when the patient is given this news she exclaims, “But how can I possibly have cancer? I just had a normal mammogram a few months ago!” Everyone is upset. The radiologist who read that “normal” mammogram a few months back (sometimes it’s only a few days or weeks before) frantically pulls up those films to see if he/she missed the cancer. Very often there was nothing on the mammogram that would have raised suspicion, yet there must have been something there since the patient now comes in a short time later with a palpable lump. How did this happen?
The answer is simple. Mammography is an imperfect test. A “normal mammogram” report does not mean that a woman does not have breast cancer. Overall, mammograms will pick up 80-90% of cancers. That’s pretty good, but there are still 10-20% of cancers that will not be seen, and will present as an “interval cancer” with a palpable lump, as in the example above.
The cancer detection rate plummets in women with dense breasts to only 40-50% of cancers picked up on a mammogram. That’s about the odds of a coin toss. This is ineffective screening by anyone’s standards.
So what is a woman over 40 to do? Find out your breast density. If you have dense breasts, you need to be especially proactive to make sure that if you do have breast cancer, you increase the odds of it being found early. Ask your doctor to send you for a screening breast ultrasound (sonogram) when you have your annual mammogram (and go to a facility that has digital mammograms).
The findings from a recent large multicenter study (ACRIN 6666) are clear:
- 7.6 cancers were found per 1000 women who had a mammogram only
- 11.8 cancers were found per 1000 women who had a mammogram and a screening sonogram
This equates to a 29% absolute increase in sensitivity by adding a screening sonogram, or an increase in the relative cancer detection rate of 50%!
Critics would argue that something might be found on the sonogram that requires a needle biopsy, and turns out not to be cancer (false positive). In my experience, most women accept the low (5%) risk of possibly having a benign needle biopsy, and don’t subscribe to the “don’t ask, don’t tell” policy when it comes to their breasts. Do yourself a favor and insist on that sonogram. Don’t take no for an answer from either your doctor or from a radiology center that tells you they don’t do screening sonograms. Seek a second opinion from another doctor. Find a radiology practice that is proactive about breast cancer screening. It’s worth your time and effort.
I’ve seen a few patients recently who have been turned away by other practices in New Jersey that won’t perform screening breast ultrasound, even though their doctor wrote them a prescription for one. Truly unbelievable, but unfortunately true. Perhaps these practices are unaware that a bill has been proposed in the NJ state legislature, which requires that women be informed of their breast density when they have a mammogram. Connecticut and Texas have passed similar bills, and the radiology practices in these states have had to accommodate the increased demand for breast ultrasounds. Bills are pending in 11 additional states, as well as at the federal level. Practices need to plan for the increased volume as women and their doctors become more aware of this important issue. (If you are at high risk for breast cancer, a breast MRI might be the better test for you; ask your doctor about this, and see “How Do I Know If I’m High Risk?”)
Be your own advocate! Your life is too important, and you only get one.
Tags: breast cancer screening, breast sonogram, early detection, high risk for breast cancer, missed breast cancer