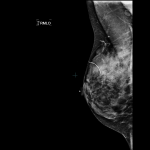
Q&A: When and How Often Should I Visit?

At what age should I start having screening mammograms, and how frequently? Why does there seem to be controversy in the media surrounding this?
- For most women, age 40 should be when you start having yearly mammograms in order to minimize your likelihood of developing advanced breast cancer. Some doctors send their patients for a baseline mammogram at age 35, and I wouldn’t argue with that.
If you have a strong family history of breast cancer (mother or sister), start having your mammogram 10 years younger than the age that relative was diagnosed, OR at age 40, whichever is younger. For example, if your sister had breast cancer when she was 44, you should start having your mammogram at age 34. If your mother had breast cancer at 60, you would start having your annual mammogram at age 40.
If you or your mother or sister have been diagnosed with the breast cancer gene (BRCA1 or BRCA2) you should begin having annual mammograms at age 25, and annual breast MRI sometimes even younger than 25. Your breast doctor should advise you on this.
If you have had Hodgkins disease (lymphoma) in the past, and were treated with radiation to your chest, you should start having annual mammograms 8 years after your treatment was completed. You should also be sent for yearly breast MRI.
As to the second part of the question: The United States Preventive Services Task Force (USPSTF), a panel appointed during the George W. Bush Administration and supported by the federal Agency for Healthcare Research and Quality, a branch of the U.S. Department of Health and Human Services, issued recommendations regarding breast cancer screening in 2009. This panel consisted of physicians in primary care (internists, pediatricians, Ob/Gyns), nurses, epidemiologists, biostatisticians, and public policy officials. Not one single breast cancer expert (breast surgeon, oncologist, radiologist, radiation oncologist) was included at the table, and there was neither invitation nor opportunity for breast cancer experts to address the panel before the recommendations were handed down. The panel recommended screening mammograms every other year, beginning at age 50; this was a significant departure from the 2002 USPSTF recommendations, which called for annual screening commencing at age 40. Incredibly, the panel also recommended that women should not be taught or encouraged to do breast self-examination, and that physicians should not perform clinical breast exams on their patients to check for cancer. Instead of being applauded as one of the few interventions in the healthcare system that actually saves people, with a 30% reduction in breast cancer mortality in the U.S. since 1991, breast cancer screening was under attack.
To support its proclamations, the panel used a computer model to create new, non-peer-reviewed data extrapolated from previously published studies on mammography screening. Some of these papers were decades old. The USPSTF used the lowest estimate of mortality reduction attributed to mammography (15%) among the various numbers that exist in the literature (as high as 54%). Even with their selective use of a low mortality reduction figure to create their new numbers, the USPSTF’s own “data” confirmed that significantly more women would survive if mammography screening began at age 40. But they ignored their own data, and they claimed that the supposed “harms” of screening (discomfort, anxiety, being called back for additional pictures, potentially having a needle biopsy that turns out to be benign, the risk of diagnosing cancers that wouldn’t necessarily kill the woman— though no one can tell us which cancers those are at the current time) outweigh the benefit of lives being saved. This was clearly not an objective, impartial scientific judgment; this was a value judgment, made with the over-arching goal of creating cost-saving public-policy recommendations for a broken healthcare system.
My advice? Start annual screening mammography at age 40; earlier if you are high risk; have a baseline at age 35 even if you are not considered high risk. The single most common cause of death among women age 35 to 50 is breast cancer. If there is any time to screen for it, it is during those years, the prime time of your life, when there are many people who need you to stick around.
Tags: annual screening, BRCA 1, BRCA 2, family history, Hodgkins, mammogram, Q&A to Honor Pink October 2012, USPSTF