What Breast Density Means to You
Breast density is one of the strongest predictors of the failure of mammography to detect cancer. About half of women younger than 50 are dense, and 1/3 of women over 50 are dense. That’s a large number of women for whom mammography alone is not enough. Up to half of breast cancers cannot be seen on the mammogram in women with dense breasts. This leads to missed cancers that are discovered at later stages, resulting in more invasive treatments and a poorer prognosis. 40,000 women in the U.S. die each year from breast cancer. Some of these women had dense breasts and didn’t know it; even though they went for mammograms every year, by the time their cancers were found it was too late. A wonderful grass-roots organization was founded by women personally affected by this lack of information (www.AreYouDense.org), and this group is doing everything it can to address this issue for all women. Because of their advocacy, laws were first passed in Connecticut and Texas, requiring that women be informed of their density when they have a mammogram. At press time for this post, 17 additional states have passed breast density inform laws: NY, NJ, PA, MA, RI, VA, MD, NC, TN, AL, HI, MO, MN, AZ, CA, NV, and OR. Bills have been introduced in SC, OH, IN, and MI. States currently working on bills: FL, ME, IL, IA, ND, CO, and WA. (For your most current state information, go to www.AreYouDenseAdvocacy.org and click on the interactive map.)
Density is determined by a mammogram. It cannot be determined with physical exam. Dense breasts have more fibrous and glandular tissue (which appear white on the films and can hide cancers, which also appear white), while breasts that are NOT dense have more fatty tissue (which appears grey and is easy to see through on the mammogram).
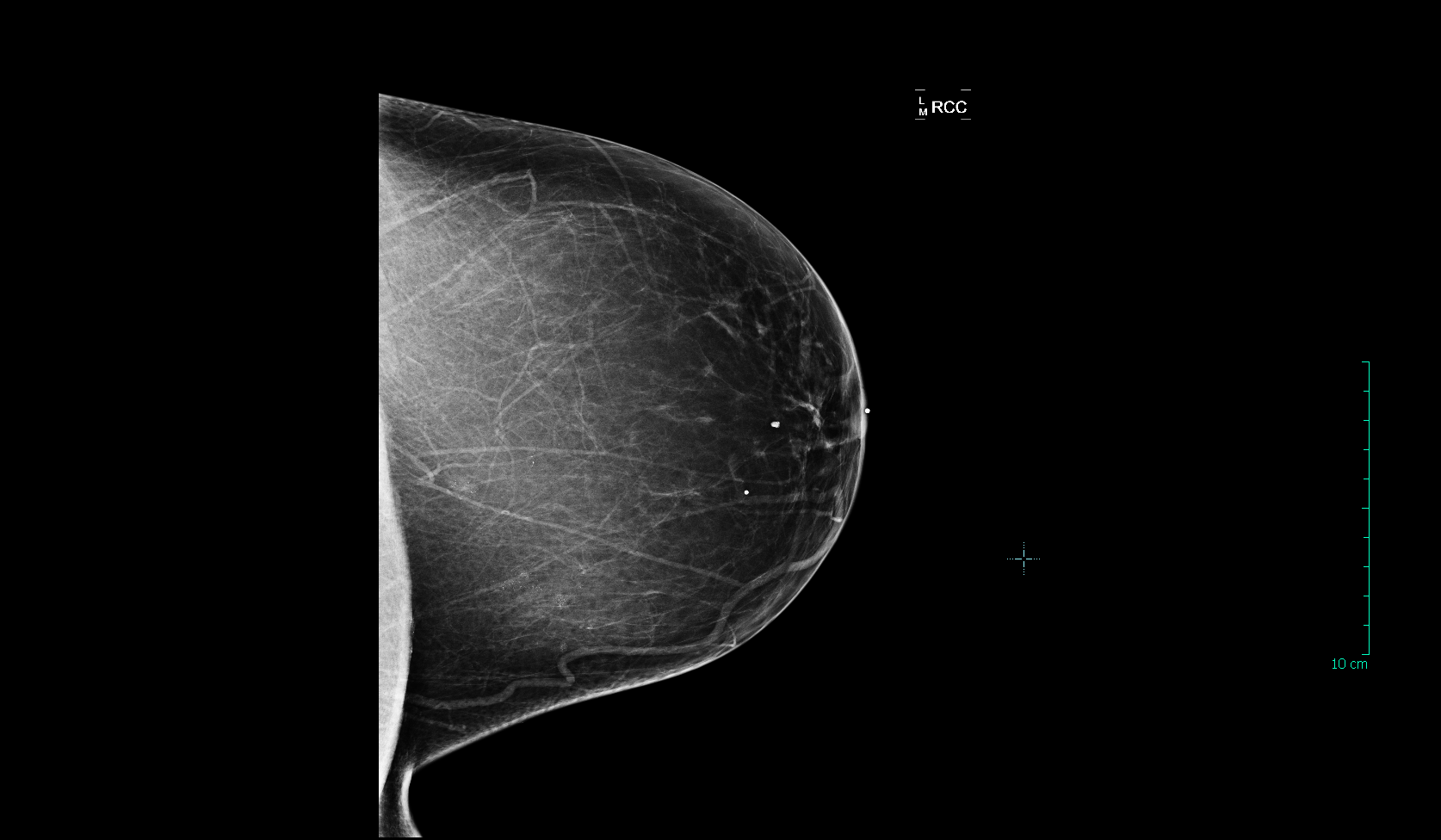
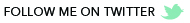
This is a mammogram view from a woman with fatty breasts that are NOT dense. The radiologist can state with a high level of confidence that there is no cancer in this breast:
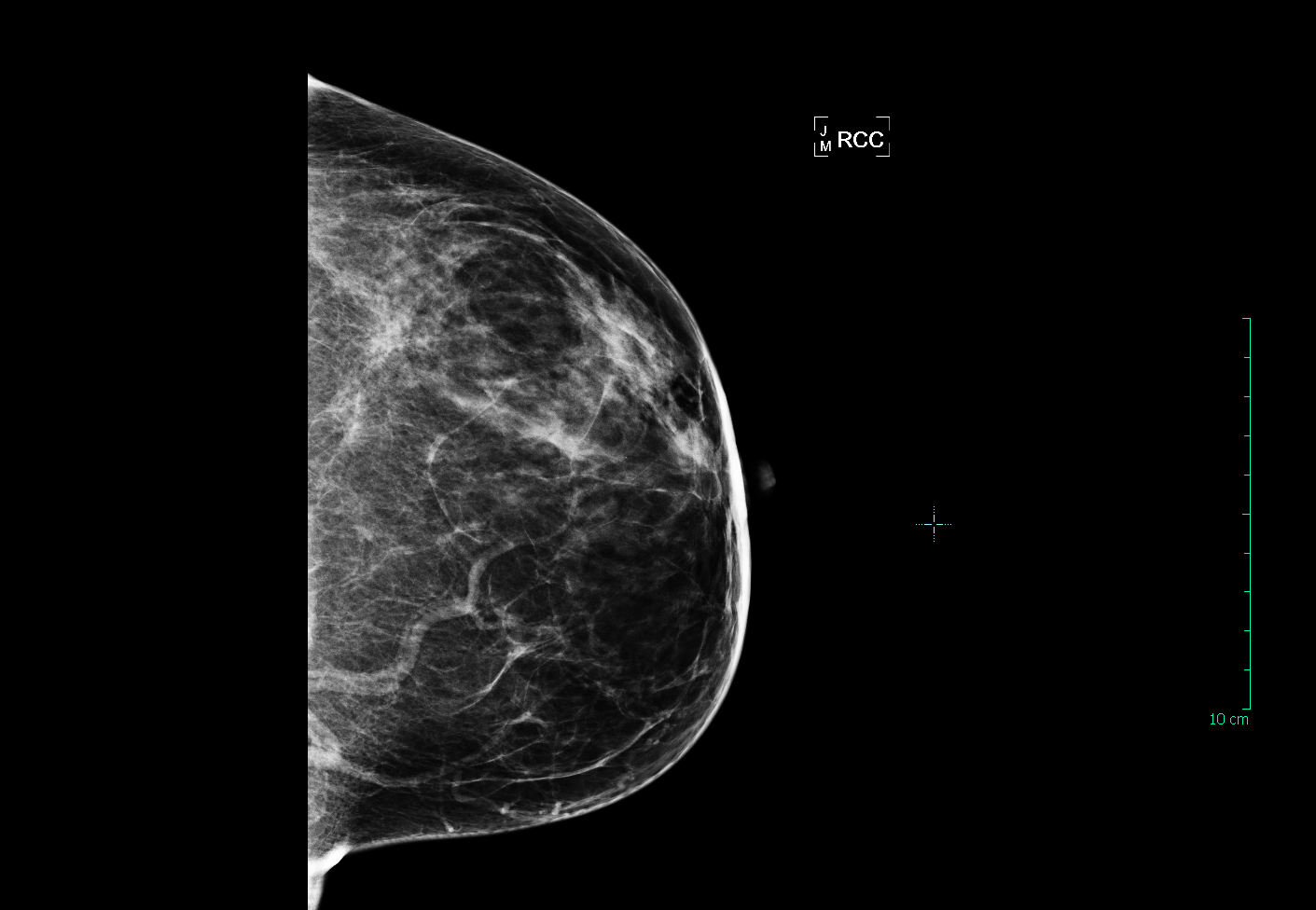
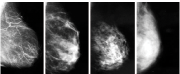
This patient has breasts that would be categorized as “scattered fibroglandular tissue”. As you can see, there is some dense white tissue on this film where cancers can potentially hide, but much of the breast is fatty and easy to see through:
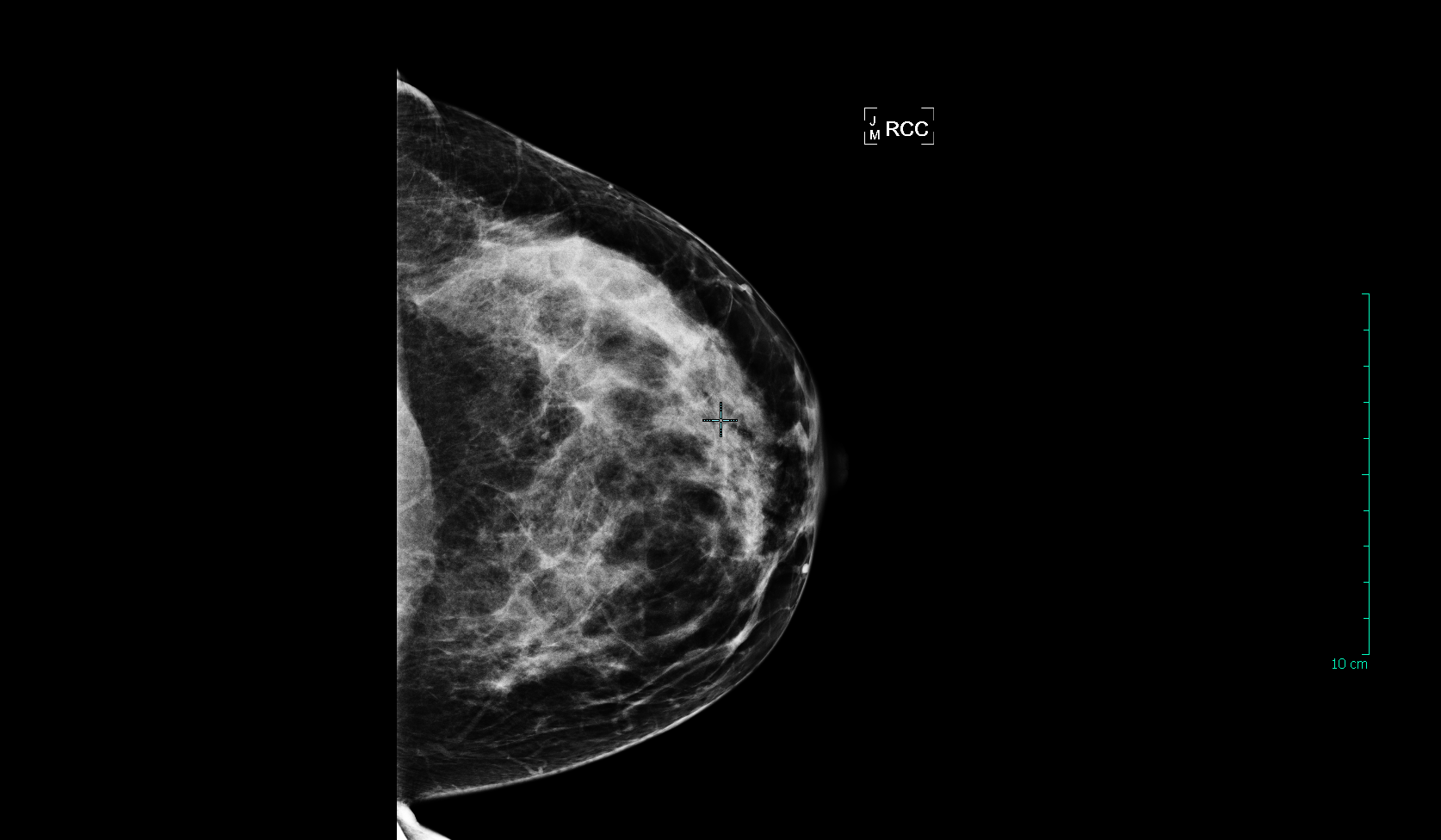
Now we start getting into the dense breasts. The patient below has “heterogeneously dense” breast tissue, which means that more than half of the tissue in her breast is dense. The ability of a mammogram to find cancer in this breast is compromised, and the patient should be sent for a breast ultrasound or MRI in addition to an annual mammogram:
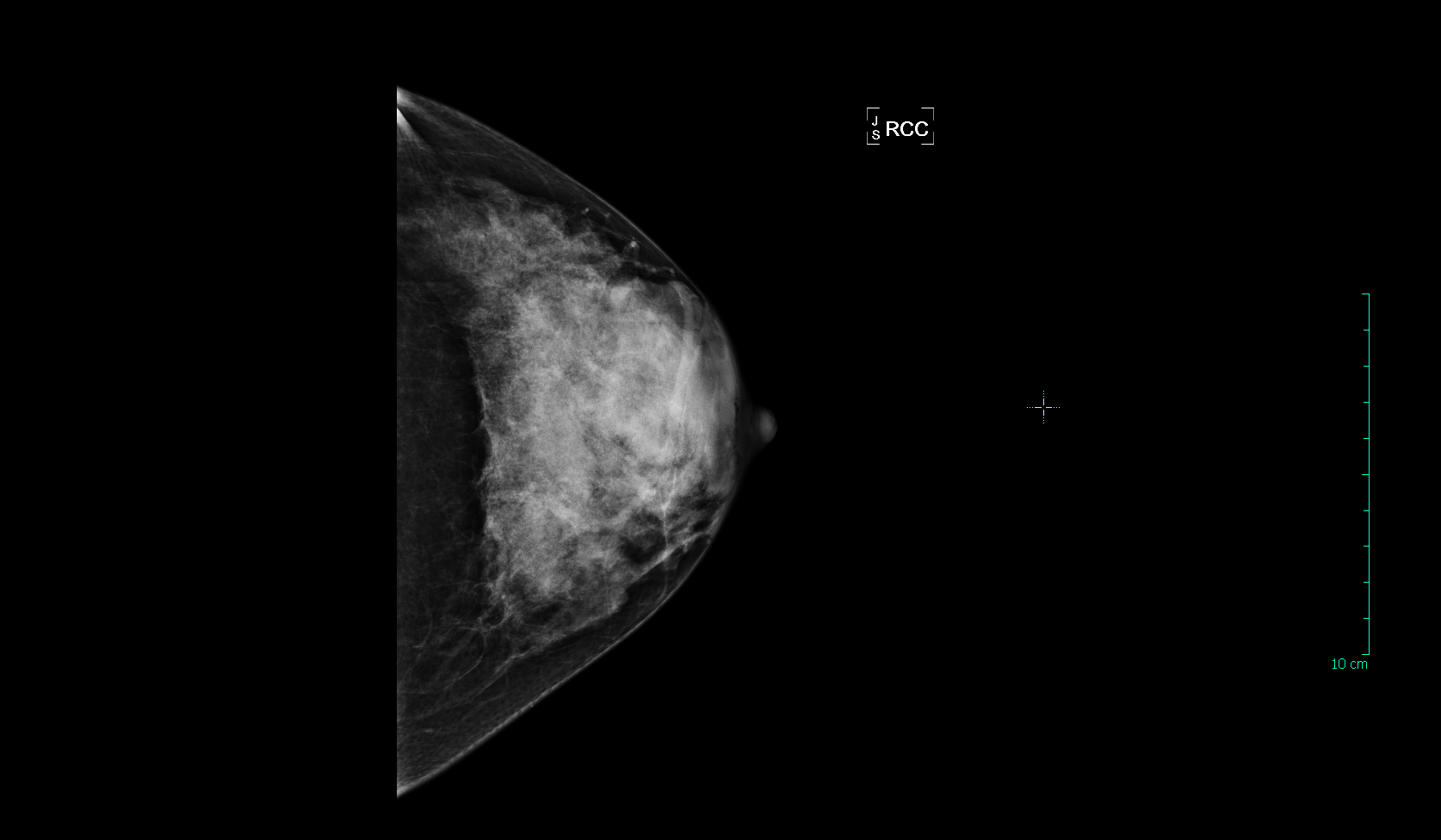
Here are two patients with “extremely dense” breasts. More than 75% of their tissue is dense, severely limiting the ability of mammography to find an early cancer. Women with breasts that are this dense also have a 4-5x greater risk of developing breast cancer compared to women with fatty (non-dense) breasts. These women should definitely be having annual breast ultrasound or MRI in addition to their yearly mammogram:
Don’t be surprised if your doctor does not know much about breast density. As the issue gains traction, the medical community will become more informed over time. For now, it is up to you to find out if your breasts are dense so you can protect yourself from advanced cancer.
Your density information should be in the official report from your mammogram, so ask your doctor for a copy of this report. Do not rely on the form letter you receive from the mammography center; this will not include your density if you do not live in one of the “inform” states. If it’s not in the official report, call the radiologist who read your films and ask him/her. It might take some legwork, but you have a right to know this! If you have “heterogeneously dense” or “extremely dense” breasts, your doctor should send you for an additional screening test each year in addition to a mammogram. If you are at high risk for breast cancer, that test should be an MRI. If you are of average risk, you should be having an ultrasound and a mammogram every year. Don’t rely on a mammogram alone, which will only find half of cancers for you! You’re taking the trouble and the time to be screened for breast cancer— Make sure that screening is effective. Your life is too important.
For more information:
www.AreYouDenseAdvocacy.org Click on the continuously updated, interactive state map on the home page to see where density legislation stands in your own state.